Expertise Reporter
 Mater
MaterFor a rustic well-known as Huge Tech’s European handle, Eire’s hospitals usually lag far behind in know-how.
They lack shared computerised affected person data, or distinctive identifiers to trace individuals once they transfer between clinics.
In July 2024, a pc system failure made Dublin’s Mater hospital push again surgical procedures and beg individuals to not come to its A&E.
Three years earlier than, Russian ransomware attackers shut down the Irish well being system’s whole pc community, and revealed 520 individuals’s medical data on-line.
However Eire now has bold targets to modernise its healthcare.
That features a programme referred to as Sláintecare. Introduced in 2017, the plan is to make use of a few of its €22.9bn (£20bn; $24bn) funds surplus to create a healthcare service that’s free on the level of care, just like the UK’s or Canada’s.
To enhance healthcare, pinch factors like diagnostics must be improved.
It is an issue being tackled at Dublin’s Mater hospital, 164-years-old and the placement of Eire’s busiest emergency division.
That is particularly so in winter, when sooner or later early this January Irish A&E departments had 444 individuals on trolleys ready to be seen.
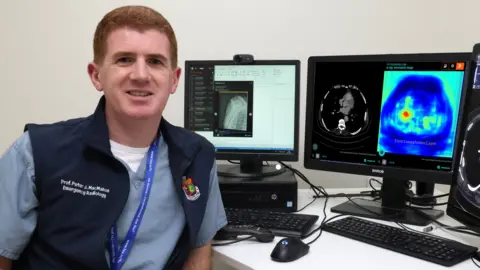
“In Eire, the massive drawback we have now is ready lists, and particularly ready for diagnostics, for MRI [magnetic resonance imaging] or CT [computed tomography] scans,” says Prof Peter McMahon, a guide radiologist on the Mater.
Due to Prof MacMahon, who as a medical scholar dabbled as a hobbyist programmer, the Mater is now among the many first hospitals in Eire to make use of synthetic intelligence (AI) throughout its radiology division – the a part of a hospital offering medical imaging to diagnose illnesses and information remedy.
To verify sufferers with essentially the most pressing wants are seen first, Prof MacMahon says: “We use AI to instantly analyse all head scans for bleeds, all chest scans for blood clots, and all bone x-rays for fractures.”
The AI is especially useful in aiding youthful medical doctors, once they do not have skilled consultants to show to.
“Now a nurse or junior physician at 2am is not alone, they have a wing man,” he says.
 Mater Hospital
Mater HospitalRural hospitals face completely different sorts of challenges.
Letterkenny College Hospital in Donegal is with out MRI amenities at evenings and weekends.
At the moment, a affected person urgently needing an MRI scan at night time can face an ambulance experience to Dublin.
However now, Prof MacMahon and the Mater’s AI analysis fellow Paul Banahan have skilled a trial AI mannequin to create a “artificial MRI” from CT scans, to instantly triage sufferers with suspected spinal accidents.
That was accomplished by feeding a “generative AI” mannequin round 9,500 pairs of CT and MRI photographs of the identical space on the identical individual.
Now the AI can predict what the MRI scan would seem like from the CT scan, one thing obtainable in all emergency departments.
And since radiology scans additionally include medical doctors’ textual content stories, he’s additionally exploring utilizing massive language fashions to establish necessary illness patterns and developments.
 Peter MacMahon
Peter MacMahonMaking use of AI to medical photographs in Eire is less complicated because the nation has saved scans in a central, digital submitting system since 2008.
However a whole lot of different necessary data, like medical notes or electrocardiograms (ECGs), stays largely in paper format in most Irish hospitals, or in smaller databases that aren’t shared centrally.
That may “severely delay” making use of AI to identify potential illnesses and enhance scientific care, factors out Prof MacMahon.
Ageing IT methods in Irish healthcare are extra broadly a problem.
“Fairly bluntly, a whole lot of hospitals are coping with legacy IT methods the place they’re simply attempting to maintain the present on the street,” says Dr Robert Ross, a senior pc science lecturer at Technological College Dublin.
“Doing the rest like integrating AI shouldn’t be straightforward to do,” he says.
Utilizing AI in healthcare shouldn’t be with out issues.
An instance right here is AI speech-recognition instruments. Utilizing them might let medical doctors spend much less time on note-taking and report writing.
However some have been discovered to make issues up, together with to invent non-existent medicine.
To stop such AI from hallucinating, “it is advisable to be certain that it is penalised in its coaching, if it provides you one thing that does not exist,” says Prof MacMahon.
AIs can have biases, however “people have biases too”, he factors out.
A drained physician, anticipating a younger affected person to be wholesome, can overlook their blood clot.
“For no matter motive we’re much more open to simply accept human error”, than in new well being know-how the place “the suitable danger is zero”, says Prof Seán Kennelly, a guide at Tallaght College Hospital and professor at Trinity Faculty Dublin.
This implies we “proceed with the phantasm of 100% accuracy in people”, and ignore areas the place AI-supported know-how could make higher scientific selections, he says.
 Tallaght College Hospital
Tallaght College HospitalHealthcare regulators, who have already got a “weak sufficient” understanding of software program as a medical machine, have not in any respect caught up with guidelines for AI, says Dr Aidan Boran, founding father of an Irish medical tech start-up referred to as Digital Gait Labs, and a researcher at Dublin Metropolis College.
For instance, getting a CE mark, which reveals {that a} medical machine meets EU security rules, consists of offering particulars in regards to the manufacturing unit the place the product is manufactured.
However within the case of software program that isn’t related says Dr Boran. “For us, manufacturing actually means copying software program,” he factors out.
AI can have a black field drawback: we will see what goes in them and what comes out, however the deep studying methods that energy these fashions are so complicated that even their creators don’t perceive precisely what occurs inside them.
That may create difficulties for a physician attempting to elucidate remedy selections that contain AI, says Dr Paul Gilligan, head of St Patrick’s Psychological Well being Providers, considered one of Eire’s largest psychological well being suppliers that runs St Patrick’s Hospital in Dublin.
When AI influences their selections, medical doctors have to “be capable of articulate the reasoning behind these selections in a fashion that’s accessible and comprehensible to these affected,” he says.

